Malaria
Malaria is a mosquito-borne infectious disease. Malaria causes symptoms that typically include fever, tiredness, vomiting, and headaches. In severe cases, it can cause jaundice, seizures, coma, or death. Symptoms usually begin ten to fifteen days after being bitten by an infected mosquito. If not properly treated, people may have recurrences of the disease months later. In those who have recently survived an infection, reinfection usually causes milder symptoms. This partial resistance disappears over months to years if the person has no continuing exposure to Malaria.
Malaria is caused by single-celled microorganisms of the Plasmodium group. It is spread exclusively through bites of infected Anopheles mosquitoes. Five species of Plasmodium can infect and be spread by humans. Most deaths are caused by P. falciparum. The mosquito bite introduces the parasites in the sporozoite form, from the mosquito's saliva into a person's blood. Sporozoites follow the bloodstream to the liver where they invade hepatocytes (liver cells) where they grow and divide. The infected hepatocytes break down and release invasive merozoites into the bloodstream. Here they invade red blood and replicate, causing lysis of the red blood cells and release of more merozoites. This results in an exponential cycle that amplifies the number of parasites in the patient's bloodstream.
Malaria is diagnosed by the microscopic examination of blood, or with antigen-based rapid diagnostic tests. The risk of disease can be reduced by preventing mosquito bites through the use of mosquito nets and insect repellents, or with mosquito-control measures such as spraying insecticides and draining standing water. Several medications are available to prevent malaria for travellers in areas where the disease is common. The recommended treatment for malaria is a combination of antimalarial medications that includes artemisinin. Resistance among the parasites has developed to several antimalarial medications. The disease is widespread in a broad band around the equator. In 2020 there were 241 million cases of malaria worldwide, resulting in an estimated 627,000 deaths.
Schistosomiasis
Schistosomiasis, also known as snail fever, bilharzia, and Katayama fever, is a disease caused by parasitic flatworms called schistosomes. The urinary tract or the intestines may be infected. Symptoms include abdominal pain, diarrhoea, bloody stool, or blood in the urine. Those who have been infected for a long time may experience liver damage, kidney failure, infertility, or bladder cancer. In children, it may cause poor growth and learning difficulty
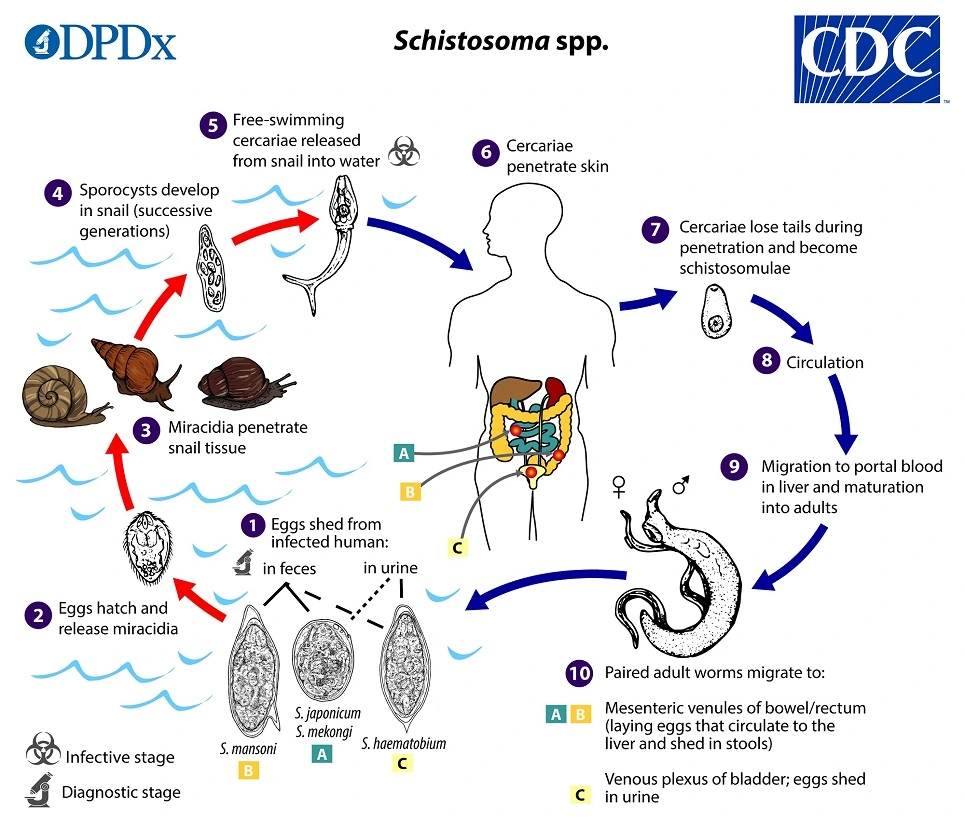
The disease is spread by contact with fresh water contaminated with the parasites. These parasites are released from infected freshwater snails. The disease is especially common among children in developing countries, as they are more likely to play in contaminated water. Other high-risk groups include farmers, fishermen, and people using unclean water during daily living. Infected Schistosoma individuals release eggs into water via their faecal material or urine. After larvae hatch from these eggs, the larvae infect specific types of freshwater snails. The schistosome larvae undergo the next phase of their lifecycles in these snails, spending their time reproducing and developing. Once this step has been completed, the parasite leaves the snail and enters the water column. The parasite can live in the water for only 48 hours without a mammalian host. Once a host has been found, the worm enters its blood vessels. For several weeks, the worm remains in the vessels, continuing its development into its adult phase. When maturity is reached, mating occurs and eggs are produced. Eggs enter the bladder/intestine and are excreted through urine and faeces, and the process repeats. If the eggs do not get excreted, they can become engrained in the body tissues and cause a variety of problems such as immune reactions and organ damage.
Diagnosis is by finding eggs of the parasite in a person's urine or stool. It can also be confirmed by finding antibodies against the disease in the blood. Methods of preventing the disease include improving access to clean water and reducing the number of snails. In areas where the disease is common, the medication praziquantel may be given once a year to the entire group. Schistosomiasis affected about 236.6 million people worldwide in 2019. An estimated 4,400 to 200,000 people die from it each year.
African Sleeping Sickness
African trypanosomiasis, also known as African sleeping sickness or simply sleeping sickness, is a parasitic infection of humans and other animals, usually transmitted by the bite of an infected tsetse fly. It is caused by the species Trypanosoma brucei. Weeks to months later, the second stage begins with confusion, poor coordination, numbness, and trouble sleeping.
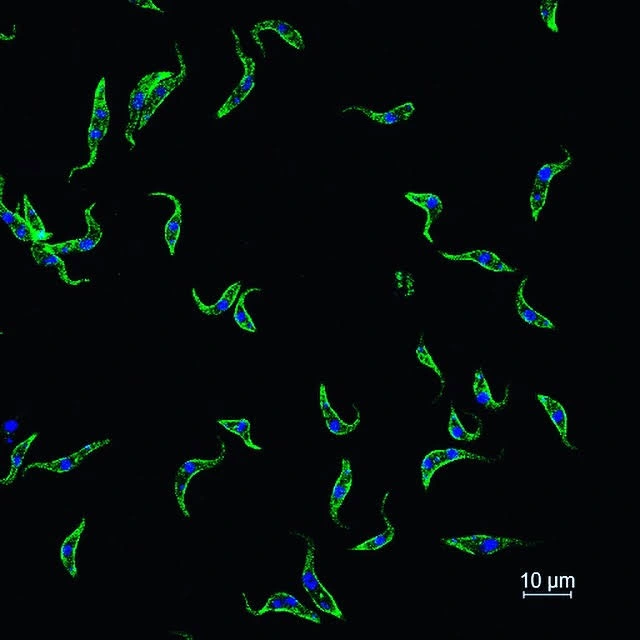
The tsetse fly serves as both a host and vector for the trypanosome parasites. While taking blood from a mammalian host, an infected tsetse fly injects metacyclic trypomastigotes into skin tissue. From the bite, parasites first enter the lymphatic system and then pass into the bloodstream. Inside the mammalian host, they transform into bloodstream trypomastigotes, and are carried to other sites throughout the body, reach other body fluids (e.g., lymph, spinal fluid), and continue to replicate.
Diagnosis is by finding the parasite in a blood smear or in the fluid of a lymph node. A lumbar puncture is often needed to tell the difference between first- and second-stage disease. If the disease is not treated quickly, it can lead to death. Prevention of severe disease involves screening the at-risk population. Treatment is easier when the disease is detected early and before neurological symptoms occur. Treatment is available but only usually effective for early infections and late stage medication has serious side effects. The disease occurs regularly in some regions of sub-Saharan Africa. An estimated 11,000 people were infected with 2,800 new infections in 2015. In 2015, it caused around 3,500 deaths, down from 34,000 in 1990.